My experience of ectopic pregnancy
Towards the end of last year I started to feel a very strange pain in my lower pelvis and had a (normally timed) period that seemed to last weeks. Now, as a woman with endometriosis, I know a thing or two about pelvic pain. But this was like a pain I’d not felt before. Combined with a strange aversion to Wednesday night’s Mexican dinner with the girls, something made me realise that something was really not right.
That Friday morning I did a pregnancy test and it was a faint positive. I wasn’t excited because I realised I might be having an ectopic pregnancy.
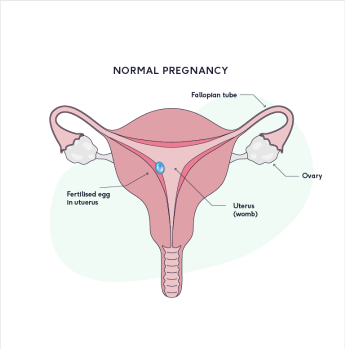
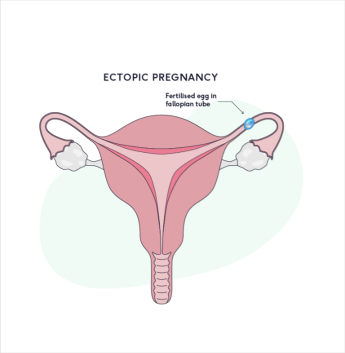
Let’s take a moment to explain what ectopic pregnancy is and how to spot it:
- An ectopic pregnancy is when a fertilised egg grows outside the womb, in the wrong place. Normally in one of the fallopian tubes.
- Unfortunately it’s not possible to save the pregnancy and it will never grow into a baby. It often has to be removed either by operation, medication or letting it pass naturally.
- Symptoms can include a combination of:
- Lower tummy pain, usually one sided
- Vaginal bleeding or spotting
- Pain in the tip of your shoulder
- Diarrhoea or loose stools
- Pain or discomfort passing urine or opening your bowels
- An ectopic pregnancy can rupture causing internal bleeding. Symptoms of this include feeling lightheaded, dizzy or faint, severe tummy pain or vomiting.
- It is potentially dangerous and in cases of rupture can be life-threatening, so if you think you may be pregnant and have any of these symptoms seek urgent medical attention like I did.
- The risk for the general population is very low – just over 1% of pregnancies are ectopic (about 1 in every 90 pregnancies)¹
- What I didn’t know is that there is some research that people who’ve had a previous infection in their fallopian tubes or endometriosis have a higher risk of ectopic pregnancy²
I rang my GP who told me to go to A&E, where I was seen ASAP. Some blood tests and ultrasounds later I was told to wait a few more days for further tests to find out what was happening. My pregnancy hormone levels weren’t so high that I needed to be rushed into surgery to have the pregnancy removed, nor were they low enough or dropping quickly enough to be a miscarriage. I was in a strange limbo.
How did I feel? On one hand I was shocked that this was happening to me, on the other not surprised at all. It feels par for the course that I will experience a whole range of women’s health issues; from having countless side effects from my contraception to being diagnosed with endometriosis. It’s safe to say I’m really not looking forward to the menopause.
Like most things in life, the reality of doing the thing you’d always imagined you would do, is so very different. Trying to get pregnant can be an immensely frustrating and confusing experience, punctuated by memories of changing sanitary towels and having logical conversations with complete strangers about your menstrual cycle.
One thing that I noticed was that whilst in hospital, three wonderful (and completely overworked) healthcare professionals asked me how many weeks pregnant I was. I really struggled to answer that question because a) I’d just found out that I was pregnant a few hours ago and had barely processed that information, and b) I didn’t really consider myself ‘pregnant’, in the sense that things were clearly not moving forward.

My Early Pregnancy Unit pre appointment questionnaire
I can now understand how difficult and confusing it must be for people who think they might be experiencing an ectopic pregnancy or miscarriage to hear this language, and wonder if there’s a better solution. Dr Mel and I agreed that perhaps asking people in my situation when their last period was might be a better way to ask the same question. I’m sure there are lots of other much more impactful examples where the medical terminology needs rethinking or reframing, and I’d love to hear your thoughts on this.
After a weekend of more tests, and then the agony of waiting 12 hours for a poor on-call Gynae registrar to call me at 10pm Sunday evening, we received the call that confirmed the pregnancy was not progressing and likely to be ectopic.
This was mainly down to pregnancy hormones. When you’re pregnant your body produces a hormone called hCG or Human Chorionic Gonadotropin; the hormone that can make some women feel nauseous.
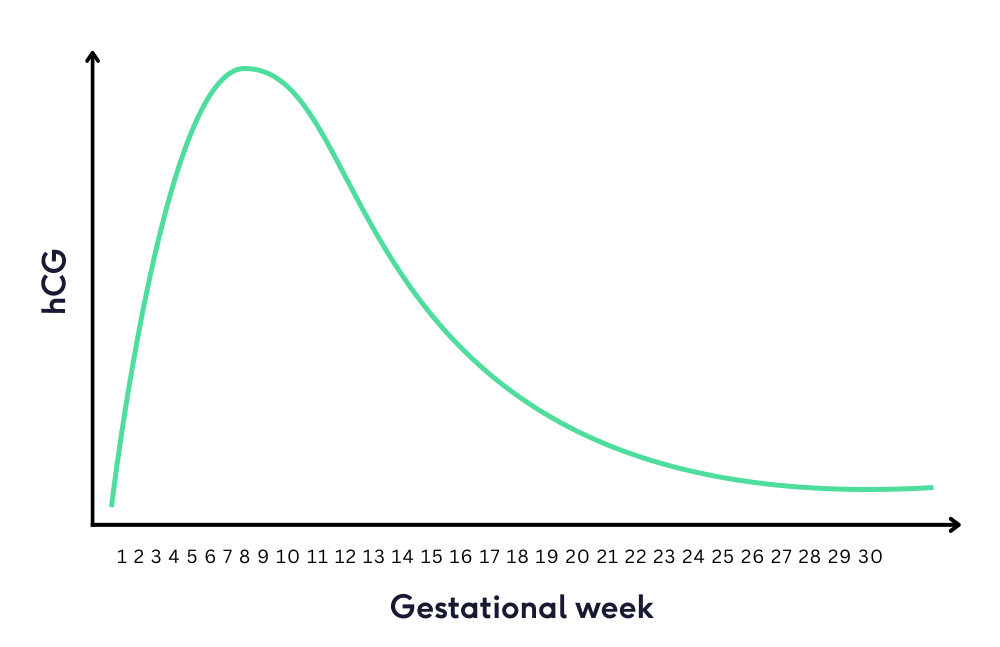
If you have suspected ectopic pregnancy or miscarriage, doctors will check your hCG levels with a blood test:
- When you’re having a progressing pregnancy, your hormone levels should roughly double every 48 hours.
- If your hormone levels drop a lot (50% every 48 hours) you’re likely to be miscarrying.
- If they drop or only rise a little bit, it’s possible the pregnancy is ectopic – or basically growing in the wrong place, and you’re going to miscarry as it won’t progress.
I was in the bracket of women whose ectopic pregnancy is managed through ‘expectant management’, which basically means you wait and see. For women who do this, between 30-100% of the time their body ends the pregnancy on its own, similar to a miscarriage.²
The news that the pregnancy wasn’t progressing hit me harder than I thought. Whilst I knew it probably wasn’t going to be good news, there was a small glimmer of hope that maybe, just maybe, the pregnancy will work out ok. I personally found this glimmer of hope almost impossible to extinguish. It’s like the monthly glimmer of hope that persuades you that your PMS symptoms are pregnancy symptoms, or that the start of your period is implantation bleeding. The glimmer of hope loves to make the wave of disappointment bigger.
I dialled into our Monday morning team call to tell The Lowdown team, and have a good cry. Naturally, I don’t understand why women should have to suffer through these things and stoically just ‘get on with it’. Today, around the world there are hundreds of thousands of women and people with vaginas dealing with unexpected, delayed or longed-not-for periods, bleeds, miscarriages and pregnancies.
Sadly, because of our society’s squeamish airbrushing of vaginas (including having strong opinions on the way they look, smell, grow hair and make sound) we make it hardest for people with vaginas to get support when they need it the most. This is the reality of our bodies, and so often it’s dusted away in this synthetic view of womanhood and motherhood. In its place is clickbait content about ‘the best sex positions when trying for a baby’.

No one is laughing and no one is eating salad
Like many, I hope that in a few years time miscarriage and baby loss become like mental health. Something that 10 years ago no one talked about, but now is part and parcel of most people’s everyday language.
One final point. The hormones are wild. The worst part for me was a week or so later when the adrenaline subsided. You wake up in your house for what feels like the 100th day in a row, and the only thing you can think about doing is making a cup of tea. You can’t exercise to lift your mood as it hurts. You can’t socialise because it feels like so much effort. You’re sick of being in the house, but equally you don’t want to leave the house. Those are the s**t days. To any of The Lowdown community reading this who’ve gone through any of these hormonal post-partum-post-miscarriage-post-anything days, I have so much empathy for what you’re going or have gone through.
If my experience was just 1000th of what it’s like to have a later or recurrent miscarriage or stillbirth, I really cannot comprehend how hard that must be to recover from. We must do better as a society and healthcare system to support and give you and your partner what you need in those moments.
Over the weeks and months that have followed, we have received some lovely emails and calls from customers telling us how much The Lowdown has helped them. These messages brought me so much happiness, and I get so much satisfaction and pleasure out of doing my dream job.
Having this experience has only spurred me on to keep improving the lived experience of what going through these things is like for us. If you’d like to share your journey with me, or tell us about your experiences of trying to conceive – I’d really love to hear from you.
Alice set up The Lowdown in 2019 with a mission to help transform the minefield that is contraception. She’s spent the last four years talking to thousands of women about this problem – and leads on the delivery of our product, brand and overall proposition.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.






