Looking after your hormonal health – choosing contraception if you’re overweight
Disclaimer: This article has been supported with an unrestricted educational grant from Exeltis UK. It has been developed independently of Exeltis, and just like all of our other content, is a completely honest breakdown. See our Content Policy for more details.
In this article
What's the lowdown?
Being overweight is medically defined as having a BMI over 25
Being in a bigger body can increase your risk of period problems like irregular periods and heavy bleeding
Symptoms and health risks associated with PCOS may be worse if you are overweight
Being overweight or obese can increase your risk of some cancers
Hormonal contraceptives can help with menstrual symptoms, reduce the risk of womb cancer and treat the symptoms of PCOS
Being in a bigger body can affect your contraceptive choice, both for ongoing contraception and emergency contraception
Progestogen-only contraceptives are a safe option if you are overweight or obese
We live in a society that is seemingly obsessed with your body weight – people love to comment on everything, whether you’re underweight, average or overweight. At The Lowdown, we want you to be happy and healthy, and that means being informed and being able to make the correct choices about your health, whatever your weight.
In this article, we discuss hormonal health and contraception if you are overweight or in a bigger body. To classify being “overweight” – medics, scientists and researchers mainly use the body mass index (BMI) calculation. We know this has flaws, but it’s an easy measure that takes into account height and weight to suggest if you are underweight or overweight. You can calculate your own BMI using the NHS calculator.
It’s important to note that people with high BMIs can still be healthy. A BMI between 20 and 25 is considered normal, 25 to 30 is considered overweight and above 30 is considered as obesity.
How can weight and body fat impact your hormonal health?
Hormonal health is a broad term that can mean many different things. In this article, we address if being overweight can cause hormonal imbalance and how a bigger body may affect your hormonal levels, periods and reproductive health.
What does oestrogen do in the menstrual cycle?
Oestrogen is produced by your ovaries and levels rise in the first part of your cycle. This causes the womb lining to thicken to allow a fertilised egg to implant into it and grow. When oestrogen levels get high enough, they trigger a hormonal cascade which releases an egg from the ovary.
Does fat produce oestrogen?
Throughout our reproductive years, the ovaries produce most of our oestrogen1. However, after we reach menopause, fat takes over the production of oestrogen in our body2,3. Women with a higher BMI have higher levels of oestrogen in their body, which researchers believe is because of the higher amounts of fat producing more oestrogen4.
Does body fat impact the menstrual cycle?
Body fat and a bigger body can impact your menstrual cycle. One study in Australia found that overweight women were more likely to have irregular menstrual cycles than women who were not overweight5. Women who were obese were twice as likely to have an abnormal menstrual cycle as women who were normal weight6. A higher BMI is also associated with heavy periods7. We still don’t know exactly why more menstrual irregularities happen in overweight women.
Being overweight, obesity and PCOS
Polycystic ovary syndrome (PCOS) is a reproductive health condition affecting around 9% of women worldwide8. One study found that 9.8% of normal weight women, 9.9% of overweight women and 9% to 12.4% of obese women have PCOS9.
Insulin resistance is a common feature in PCOS. This is where the body’s cells become less responsive to insulin, a hormone that helps regulate blood sugar levels. If women with PCOS gain weight, the associated insulin resistance becomes more severe10,11, and it’s the insulin resistance that is linked to health problems like diabetes and high cholesterol12.
People with PCOS experience varying symptoms but the condition is characterised by irregular periods, excess levels of the androgen hormones (leading to symptoms like acne, oily skin and excess hair) and follicles that look like cysts on the ovaries. We know that if you lose weight, PCOS symptoms can improve13. Contraceptives can also be an excellent way to help manage the symptoms of PCOS.
Being overweight and cancer
Breast cancer
Breast cancer affects 1 in 7 women in their lifetime14. There are several known risk factors for breast cancer, which include age, family history, being overweight or obese and using hormonal contraceptives or hormone replacement therapy15.
As we’ve learnt, having more body fat is associated with higher levels of oestrogen, which may partly explain the link between breast cancer risk and being overweight16. In fact, researchers believe that many of the risk factors for breast cancer are due to their link with increasing sex hormone levels in the body17.
Endometrial (womb) cancer
Most womb cancers are driven by oestrogen which encourages the inner lining of the womb to grow and thicken excessively18. 34% of womb cancers in the UK are caused by being overweight or obese19, which is thought to be due to the higher levels of oestrogen caused by increased body fat20.
Using hormonal contraception including the pill or coil can reduce your risk of womb cancer21,22. This is because hormonal contraception contains progestin, a synthetic form of the hormone progesterone which prevents the womb lining thickening.
Weight and contraception
Choosing the right contraceptive for your weight
The best contraception for overweight women or best contraception for obese women is individual and takes into account both what you want to use, and how safe a method is for you.
Risks of hormonal contraception if overweight
If your BMI is over 30 and you use combined hormonal contraception (like the combined pill, patch or ring), this can increase your risk of blood clots and cardiovascular disease compared to if your BMI is less than 3023. This is why it’s important to discuss your choice with a healthcare professional who will help weigh up all the risks and benefits of each method to get the best choice for you. Our recommender tool is a great place to start.
If you have a BMI over 30 and use the contraceptive injection, this can be associated with weight gain in some women.
However, if you use progestogen-only contraception such as the progestogen-only pill, implant or hormonal coil there is no increased risk of blood clots or heart disease if your BMI is over 30, compared to users with a BMI under 30.
Generally this means:
- If you have a BMI of 25 to 35 and no other medical problems, you can choose any method of contraception24.
- If your BMI is between 30 and 35, and you have other risk factors for heart disease (like high cholesterol, smoking and diabetes) or blood clots, OR if your BMI is above 35, you are advised to avoid combined hormonal contraception and the contraceptive injection25. In these cases it is recommended to use progestogen-only or non-hormonal contraception26.
Benefits of hormonal contraception if overweight
If you are overweight, you are more likely to have problems with your periods as we’ve discussed above. Hormonal contraception can make periods lighter, less frequent, less painful or stop altogether. Combined contraception can regulate periods and make them lighter, or you can use it to avoid having a monthly bleed altogether. Even if you can’t have combined hormonal contraceptives, progestogen-only contraception can still help manage period symptoms.
Furthermore, both combined and progestogen-only contraception can reduce the risk of womb cancer which is important if you are overweight, obese or have PCOS27,28.
Does being overweight make contraception less effective?
Contraceptives which are effective at all weights and BMIs include:
- The combined pill
- The vaginal ring
- The progestogen-only pill
- The implant
- The contraceptive injection
- Hormonal and copper coils
The patch may be less effective if you weigh over 90kg so the manufacturer recommends choosing a different method29. The risk of a coil falling out (expulsion) is around 1 in 20, however this increases in your BMI is over 25 and increases as BMI gets higher. If your BMI is over 40, the risk of expulsion is twice as high30.
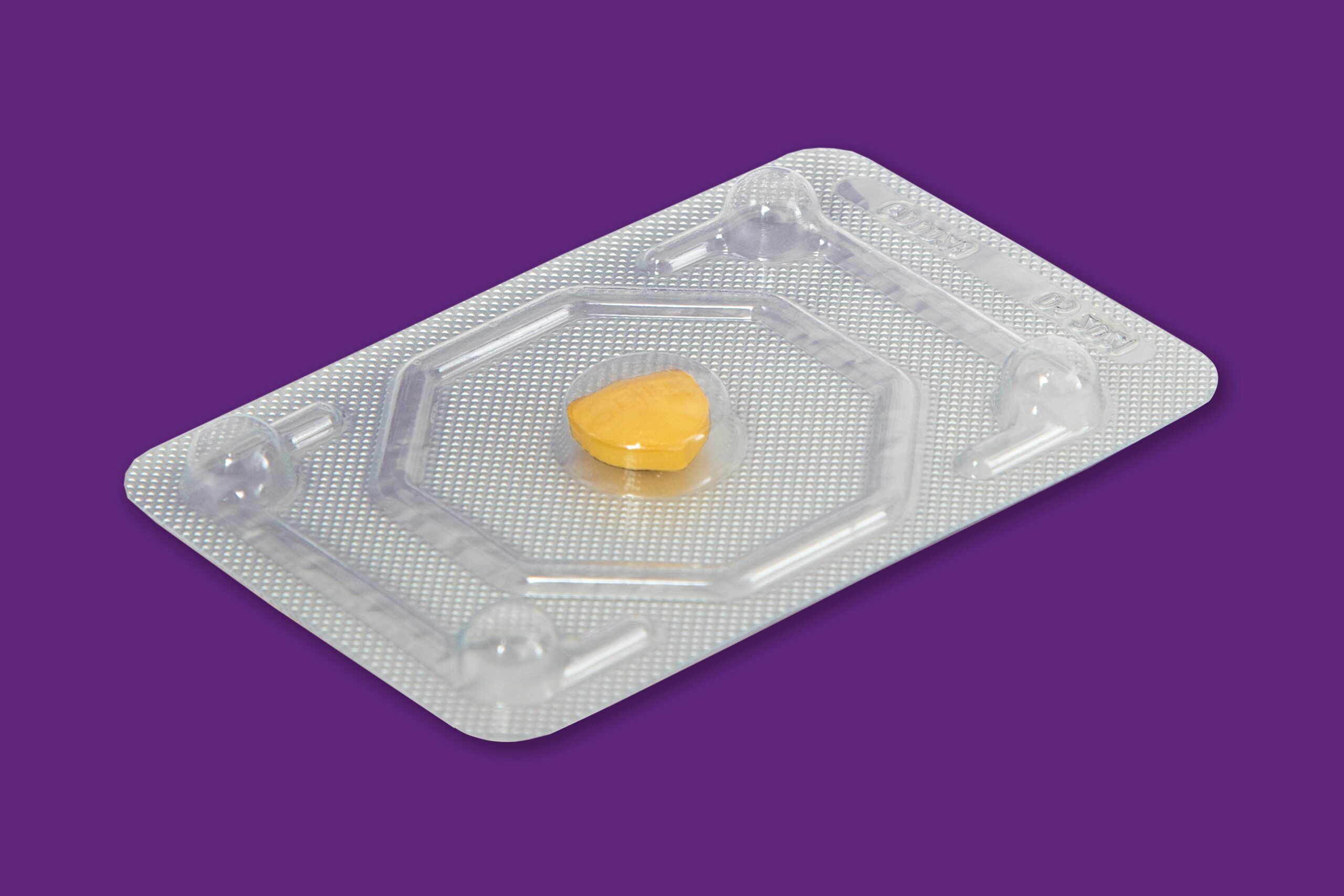
Is the morning after pill less effective if overweight?
Although there has been some research, there isn’t enough to say whether the morning after pills are less effective if you are overweight or obese31. However, guidelines are cautious and if you are over 70kg or have a BMI of 26 or above, you should be offered two levonorgestrel tablets if this is the pill you choose32.
The copper coil is the most effective form of emergency contraception, regardless of weight or BMI.
Weight loss injections and contraception
The invention of weight loss injections – known as GLP-1 agonists – has led to people choosing to use these to control their weight and BMI.
Ozempic and contraception
Ozempic and Wegovy (brand names for semaglutide) do not affect your contraception.
Mounjaro and contraception
However, Mounjaro (brand name for tirzepatide) may reduce the effectiveness of oral contraceptives33. It’s advised to switch to a form of contraception that you don’t have to swallow, or to use condoms for the first four weeks of using Mounjaro and for four weeks after each dose change23.
Being overweight or in a bigger body should not stop you from having a discussion about your contraceptive choice. You have many options and at The Lowdown we believe everyone should be educated and listened to make the best decision for their reproductive health.
Our medical review process
This article has been medically reviewed for factual and up to date information by a Lowdown doctor.